Cervical cancer
Find a doctorCervical cancer affects the lower part of the uterus, called the cervix. At Atrium Health Floyd and Harbin Clinic, our cancer specialists provide advanced treatments for all types and stages of cervical cancer.
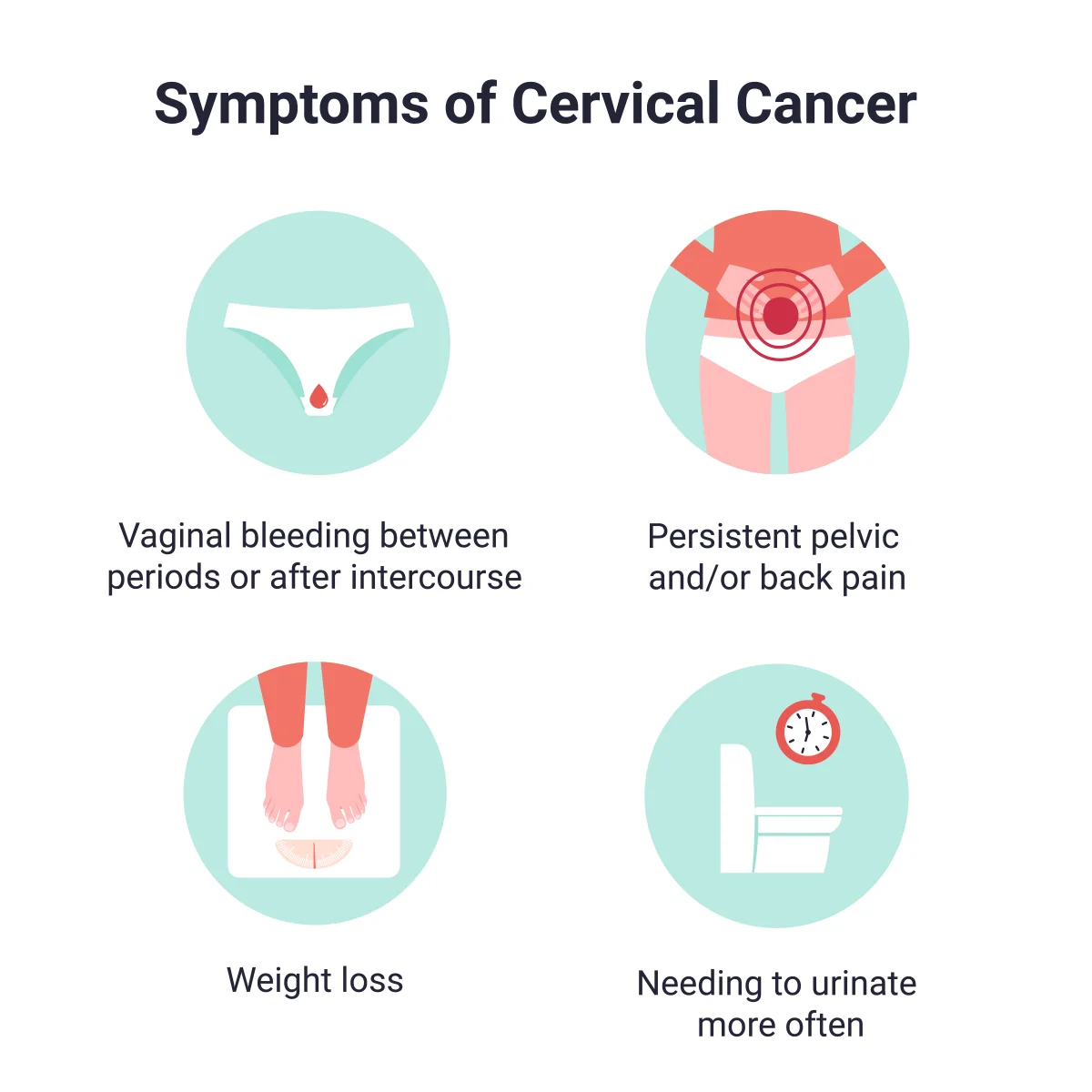
Different signs of cervical cancer.
What is cervical cancer?
Cervical cancer occurs when cells in the lining of the cervix change and grow uncontrollably. The cervix is the lower part of the uterus (womb). It connects the upper part of the uterus to the vagina.
Causes of cervical cancer
A sexually transmitted infection (STI) called human papillomavirus (HPV) causes most cases of cervical cancer. HPV is a common STI with different virus strains or types. Depending on the strain, you may develop genital warts, cervical cancer or no health issues.
Many people with HPV don’t know they have the virus. Their body fights off the virus without causing symptoms or long-term problems. Cervical cancer occurs when the virus turns off tumor-suppressing genes that help prevent cancer. Cells lining the cervix then begin to change and rapidly multiply.
Cervical cancer symptoms
Common signs of cervical cancer include:
- Painful sex
- Periods that last longer or are heavier than usual
- Unusual vaginal bleeding after sex, between periods or after menopause
If cervical cancer becomes more advanced, you may develop these symptoms:
- Bone fractures
- Diarrhea or blood in your stool
- Fatigue
- Painful urination or blood in your urine
- Pain in your back, pelvis or legs
- Swollen legs
- Unintentional weight loss
Cervical cancer types
Doctors determine the type of cervical cancer based on how the cells look under a microscope. Types of cervical cancer include:
- Squamous cell carcinoma: Most cervical cancers are squamous cell carcinomas. Cancer forms in flat cells that line the outer surface of the cervix (ectocervix).
- Adenocarcinoma: This type of cervical cancer starts in ectocervix cells that make mucus (glandular cells).
- Mixed (adenosquamous) carcinoma: Less commonly, cervical cancer is a combination of squamous cell carcinoma and adenocarcinoma.
Cervical cancer diagnosis
Cervical cancer often starts as a precancerous condition called cervical dysplasia. A Pap test, which is part of a women’s health exam, can detect dysplasia. Also called a Pap smear, this test looks for changes to cervix cells.
If your Pap test result is abnormal, your doctor may perform other tests, including:
- HPV test to check for viral strains that cause cervical cancer
- Colposcopy, using a scope device to view the cervix and remove a tissue sample to look at under a microscope
If these tests indicate colorectal cancer, further testing can help doctors determine whether the cancer has spread outside the cervix. Your doctor may order tests such as:
- Cystoscopy, using a scope device to view and take tissue samples from the bladder and urethra
- Imaging tests, such as CT scan, MRI and positron emission test (PET) scan, to find out whether the cancer has spread to organs and bones
- Proctoscopy, using a scope device to view inside your rectum
Cervical cancer staging
Cancer staging reflects whether the cancer has spread and helps doctors make treatment decisions. Each stage of cervical cancer has distinct substages. The four main stages of cervical cancer include:
- Stage 1: Cancer is only in the neck of the cervix lining and hasn’t spread.
- Stage 2: Cancer has spread outside the cervix and uterus. It hasn’t spread to the pelvic walls, lower part of the vagina or nearby lymph nodes.
- Stage 3: Cancer has spread to the pelvic walls or lower part of the vagina. Cancer may or may not affect nearby lymph nodes. A tumor may block the ureter tubes that carry urine from the kidneys to the bladder.
- Stage 4: Cancer has spread into the bladder, rectum or distant organs like the lungs or bones.
Cervical cancer risk factors
An HPV infection is the main risk factor for cervical cancer. Other factors that can increase your risk include:
- Being sexually active before age 18
- Family history of cervical cancer
- Having multiple sexual partners
- Human immunodeficiency virus (HIV)
- Long-term use of birth control pills (oral contraceptives)
- Not getting regular Pap tests
- Smoking
- Weakened immune system
Cervical cancer prevention
Actions that may help lower your chances of developing cervical cancer include:
- Getting the HPV vaccine
- Limiting your number of sexual partners
- Seeing your primary care provider or OB-GYN for regular Pap tests
- Seeking help to quit smoking
- Using condoms and dental dams during sex
Cervical cancer treatments
Cervical cancer treatments depend on your cancer stage, symptom severity and overall health. Surgery is a common treatment for cervical cancer. Surgical options include:
- Conization, using a laser beam, surgical blade or wire heated by electricity (loop electrosurgical excision procedure or LEEP) to remove a cone-shaped piece of tissue from the cervix
- Cryotherapy, using extremely cold temperatures to freeze and destroy cancer cells
- Laser ablation, using a laser beam to burn and destroy abnormal tissue
Treatments for advanced stages of cervical cancer may include:
- Chemotherapy to destroy cancer cells throughout the body
- Hysterectomy to surgically remove the cervix and uterus
- Radical hysterectomy to surgically remove the cervix, uterus, upper part of the vagina and pelvic lymph nodes
- Pelvic exenteration, a complex surgery to remove all pelvic organs, including the bladder and rectum
- Radiation therapy, including external radiation therapy and brachytherapy, to kill cancer cells
Cancer services
Personalized cancer care from experts you trust
Get the MyAtriumHealth app
Get test results, message your provider & more.