I’m in my 30s
While you may be a few years away from needing a screening mammogram, there are measures you can take in your 30s for your breast health. Choose from the personalized tips below to learn more about breast health in your 30s.
Know preventative care guidelines
An annual screening mammogram is not usually necessary yet, but the National Comprehensive Cancer Network suggests having a clinical breast exam every one to three years. This hands-on exam performed by a trained provider will give you invaluable knowledge about your unique breasts.
The visit should also include family and personal health and cancer history to determine your risk. If you have a family history of breast cancer, your provider might recommend a baseline mammogram before the age of 40.
Now is the time to develop healthy exercise and eating habits. As you age, obesity increases your risk of developing breast cancer.
Know mammograms
While you may be a few years away from needing a screening mammogram, it is time to understand when a mammogram might be needed in your breast health.
If you begin experiencing breast pain, nipple discharge or a lump, your health care provider might recommend a diagnostic mammogram. This low-radiation X-ray of the breast provides images of your breast tissue and helps a radiologist examine your breast issue.
In your 30s your breast tissue is still dense, which makes X-rays more difficult. 3D imaging has enhanced mammogram technology to provide a detailed, layer-by-layer images of breast tissue even when it is still dense.
Know breast pain
At 30, you’re no stranger to breast pain or tenderness caused by hormone fluctuations. If a new pain appears, consider these potential reasons:
- Bra: An unsupportive or too tight-fitting bra can cause breast aches and pains.
- Pregnancy: Swollen, achy breasts are often the first signs of pregnancy due to hormone changes.
- Breastfeeding: If a milk duct becomes blocked, you could experience a painful infection called mastitis.
- Exercise: Running and upper body exercises can make the muscles behind your breast sore.
- Caffeine: Caffeine causes blood vessels to dilate, which can make breasts swell and feel painful.
If you feel a lump, you might keep an eye on it through one menstrual cycle. If it goes away, then it was probably hormonal. But if the lump doesn’t go away, be sure to have it checked out.
Know clinical breast exams
The National Comprehensive Cancer Network suggests women in their 30s have a clinical breast exam every one to three years. This hands-on clinical breast exam is performed by a trained provider and can identify some cancers undetected by mammography.
Some questions to ask your provider during the exam include:
- How can I tell the difference between my usual lumps and lumps I need to do something about?
- How will you be able to tell what kind of breast change I have?
- What should we do to watch this change over time?
The visit should also include family, personal health and cancer history to determine your risk.
Know your breast
You might notice your breasts feeling softer in your 30s, and the color of your nipples can change during pregnancy.
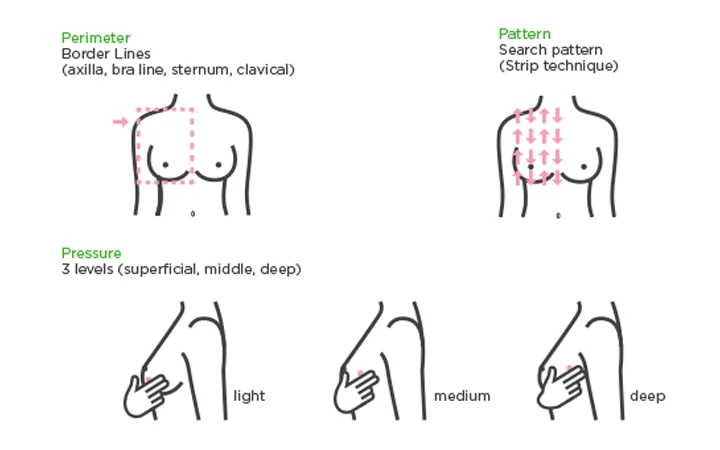
Take the time for breast awareness and follow the three Ps:
- Perimeter: Using the pads of your middle three fingers, trace from your collarbone to your armpit, down the outside of your breast, underneath and then back up to your collarbone again.
- Pattern: Beginning under your arm, move your fingers in straight vertical lines over your breasts.
- Pressure: Move the pads of your fingers in small, dime-size circles over your breast tissue and underarms, using light, medium and deep pressure.
Take note of discharge from your nipples and itchy, red or scaly skin. If you find a rock-like lump, call your physician. If you find soft lump, keep track of it. If it doesn't go away after your next period, call your doctor. Eighty percent of lumps biopsied are not cancerous. But any new, persistent lump should be evaluated.
Know risk factors
The more you know about your body and your family history, the more empowered you are to determine your breast cancer risk. Have your risk assessed during your clinical breast exam. If your health care provider determines you are high risk, you might begin having mammograms before the age of 40.
Risk is determined by factors including:
- Genetic risk: When genetic defects are passed down in your genes from your parents.
- Familial risk: Cancer has been diagnosed in your family but it might be linked to environmental or lifestyle factors, not your genes.
- Personal risk: Unique to you modifiable risks, such as alcohol consumption, lack of exercise, smoking, unhealthy diet, and non-modifiable risks, such as breast density, late menopause and previous radiation therapy of the chest wall.
Get to know your family history by asking questions such as who had cancer, what type of cancer and at what age were they diagnosed. Be sure to share this information with your health care provider.
Know your genes
Approximately 10 to 15% of all breast cancers are inherited. This makes knowing your family history key to understanding your risk. Genetic mutations can be passed down, and science has shown a BRCA mutation is the single, biggest risk factor for breast cancer.
You may want to consider genetic counseling and testing if your family medical history includes:
- You're a female who was diagnosed with breast cancer before the age of 50
- You’re a male who was diagnosed with breast cancer or you have a close male relative who was diagnosed with breast cancer
- You have a mother, sister, daughter, grandmother or aunt who had breast cancer before age 50 or ovarian cancer at any age
- You have three relatives on the same side of the family who were diagnosed with breast cancer at any age
