I’m in my 40s and 50s
When you’re in your 40s, it’s time to begin scheduling annual mammograms. In your 40s and 50s, you might even notice some changes in your breasts as your body begins to transition towards menopause. Learn more about your breast health during this time by choosing from the personalized tips below.
Know preventative care guidelines
Starting at age 40, you should schedule a screening mammogram every year, according to the National Comprehensive Cancer Network. It is the best tool available in the early detection of breast cancer.
And don't stop when you turn 50. About 75% of all breast cancer cases occur after the age of 50, so it’s important that you continue to be vigilant about your breast health.
In addition, you should also have an annual clinical breast exam. This hands-on exam performed by a trained provider will give you invaluable knowledge about your unique breasts. The visit should also include risk assessment.
If you have reached menopause, you may notice new lumps. That is not a reason to panic. Those lumps can often be cysts. Make sure to talk to your doctor if any new lumps are found.
Know mammograms
Mammogram should be a familiar word starting in your 40s. According to the National Comprehensive Cancer Network, this is the age women should have a screening mammogram every year.
The X-ray of your breast is likely to cause some discomfort. Here are some tips to help reduce the discomfort:
- Schedule a week after your menstrual period
- Consume less caffeine to reduce tenderness
- Take a nonsteroidal anti-inflammatory drug such as ibuprofen an hour before your mammogram
- During the mammogram, take slow, deep breaths to reduce tension-induced pain
Advances in breast health technology are providing radiologists with more detailed images even on dense breast tissue. 3D mammography now provides detailed, layer-by-layer images of breast tissue.
Know breast pain
As your body begins to transition towards menopause, your breast can feel more tender or even more lumpy. Tracking your pain with your cycle to identify patterns can still be a helpful way to find your normal. As your hormone levels become irregular, here are three common changes you might notice:
- Cup size: Changes in estrogen can cause breast to change sizes. You might need to change bra sizes to get a proper, pain-free fit.
- Fibrocystic breast: If you haven't had fibrocystic lumps, you might begin to feel them.
- Mammary duct ectasia: Breast ducts can become swollen and clogged, causing pain and nipple discharge.
Breast cancer doesn't typically present as pain or pain in both breasts. After menopause, it is common for women to stop having lumps, pain and nipple discharge.
Know clinical breast exams
The National Comprehensive Cancer Network suggests women in their 40s and 50s get a clinical breast exam and a screening mammogram every year. Your cancer risk steadily increases with age.
This hands-on clinical breast exam is performed by a trained provider. The exam can identify some cancers undetected by mammography.
There are some questions you should ask your provider about a breast change:
- How can I tell the difference between my usual lumps and lumps I need to do something about?
- How will you be able to tell what kind of breast change I have?
- What should we do to watch this change over time?
Getting to know your family health and cancer history will help determine your risk.
Know your breast
The combination of menopause, weight gain and age can cause your breasts to both swell and become less dense in your 40s and 50s. Lumpiness due to non-cancerous fibrous tissue can also occur.
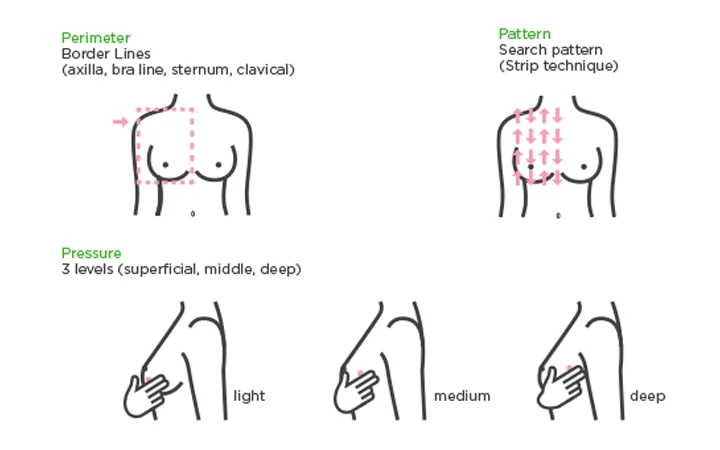
Take the time for breast awareness and follow the three Ps:
- Perimeter: Using the pads of your first three fingers, trace from your collarbone to your armpit, down the outside of your breast, underneath and then back up to your collarbone again.
- Pattern: Beginning under your arm, move your fingers in straight vertical lines over your breasts.
- Pressure: Move the pads of your fingers in small, dime-size circles over your breast tissue and underarms, using light, medium and deep pressure.
Be sure to take note of discharge from your nipples and itchy, red or scaly skin. While 80% of lumps biopsied are not cancerous, it’s a good idea to have any new lump checked by your health care provider.
Know risk factors
Age begins to play a role in your risk for breast cancer starting in your 40s. If you haven't been to a health care provider for breast screening, you should receive a risk assessment during your first visit for a mammogram.
Breast cancer risks are grouped into three broad categories:
- Genetic risk: These are genetic defects passed down in your genes from your parents.
- Familial risk: This is a cancer diagnosis in your family but it might be linked to environmental or lifestyle factors, not your genes.
- Personal risk: These risks unique to you includes things you can control, such as alcohol consumption, lack of exercise, smoking and an unhealthy diet. It also includes non-modifiable risks, such as breast density, late menopause and previous radiation therapy of the chest wall.
When talking to your family, ask if anyone had cancer. If the answer is yes, find out what type of cancer and how old they were when diagnosed. Then share this information with your health care provider.
Know your genes
Approximately 10 to 15% of all breast cancers are inherited. That’s why knowing your family history is more than just helpful – it’s essential.
Some genetic mutations can be passed down to family members. Among them, BRCA mutation is considered the biggest risk factor for breast cancer. Identifying this risk factor early can help you take steps for prevention and early detection of breast cancer.
Talk to your health care provider if genetic testing might be right for you, especially if your family history includes:
- You're a female who was diagnosed with breast cancer before the age of 50
- You’re a male who was diagnosed with breast cancer or you have a close male relative who was diagnosed with breast cancer
- You have a mother, sister, daughter, grandmother or aunt who had breast cancer before age 50 or ovarian cancer at any age
- You have three relatives on the same side of the family who were diagnosed with breast cancer at any age
