I’m in my 60s or older
Turning 60 is no reason to stop having an annual breast exam or mammograms. Your chances of getting breast cancer steadily increase with age, according to the National Cancer Institute.
Learn more about your breast health in your 60s and beyond by choosing from the personalized tips below.
Know preventative care guidelines
For 80% of breast cancer patients, the only risk factors are age and gender. That is why it is important that you continue to take charge of your breast health even if you’re in your 60s or older. You may notice your breasts becoming less lumpy; that is normal with age.
A mammogram remains the best screening tool available in the early detection of cancer, and you should be getting one annually, according to the National Comprehensive Cancer Network. You should also have an annual clinical breast exam. This hands-on exam performed by a trained provider will give you invaluable knowledge about your unique breasts. The visit should also include risk assessment.
Know mammograms
It's a common myth that when you reach 60 you no longer need an annual screening mammogram. But women in their 60s who have regular mammograms have a less risk of dying from breast cancer than those who aren't screened.
If you haven't had a mammogram recently, technology has improved. 3D mammography now offers multiple images of breast tissue from many different angles which reduces the likelihood of getting called back for more mammographic images
Know breast pain
Breast pain might be less common but still occurs in menopause. Sometimes pain in your 60s is linked to hormone replacement therapy and lifestyle factors that cause swelling. Every woman is different but the common triggers are:
- Anatomical factors, such as cysts, trauma or surgery
- Hormone replacement therapy
- Stress
- Mastitis
- Dietary triggers such as caffeine, salt, fatty foods, alcohol
Mammograms continue to be key to understanding any breast pain that persist.
Know clinical breast exams
Your cancer risk steadily increases with age, so 60 is not time to stop being proactive about your breast health. You should continue getting an annual clinical breast exam along with a mammogram.
This hands-on clinical breast exam is performed by a trained provider to help identify some cancers undetected by mammography.
There are some questions you should ask your provider about a breast change:
- How can I tell the difference between my usual lumps and lumps I need to do something about?
- How will you be able to tell what kind of breast change I have?
- What should we do to watch this change over time?
Know your breast
In this stage of life your breasts will lose some of their firmness. The good news is that an annual mammogram will be more effective in detecting a tumor. Lumpiness due to non-cancerous fibroid tissue can also occur.
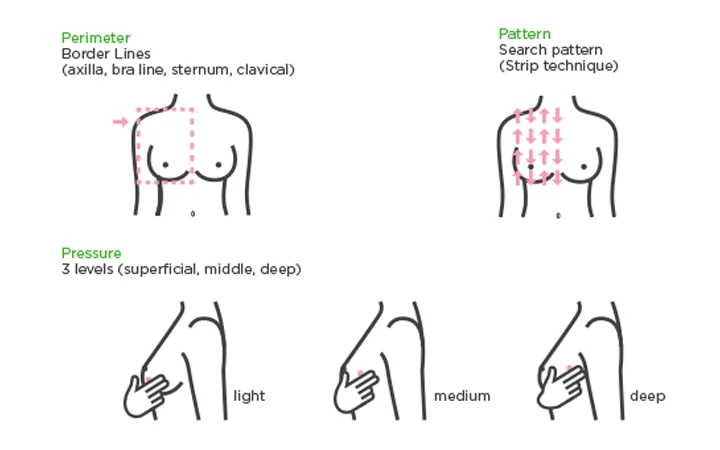
Take the time for breast awareness and follow the three Ps:
- Perimeter: Using the pads of your first three fingers, trace from your collarbone to your armpit, down the outside of your breast, underneath and then back up to your collarbone again.
- Pattern: Beginning under your arm, move your fingers in straight vertical lines over your breasts.
- Pressure: Move the pads of your fingers in small, dime-size circles over your breast tissue and underarms, using light, medium and deep pressure.
Take note of discharge from your nipples and itchy, red or scaly skin. While 80% of lumps biopsied are not cancerous, it’s a good idea to have any new lump checked by your health care provider.
Know risk factors
Your risk for breast cancer increases as you age, even into your 60s. If you haven't been to a health care provider for breast screening, you should receive a risk assessment during your first visit for a mammogram.
Breast cancer risks are grouped into three broad categories:
- Genetic risk: These are genetic defects passed down in your genes from your parents.
- Familial risk: This is a cancer diagnosis in your family but it might be linked to environmental or lifestyle factors, not your genes.
- Personal risk: These are risks unique to you. Modifiable risks are things you can control, such as alcohol consumption, lack of exercise, smoking and an unhealthy diet. There also are non-modifiable risks, such as breast density, late menopause and previous radiation therapy of the chest wall.
Get to know your family history. Ask questions about who had cancer, type of cancer and what age they were they diagnosed. Share this with information with your health care provider.
Know your genes
Approximately 10 to 15% of all breast cancers are inherited. This makes knowing and sharing your family history key.
Genetic mutations can be passed down. Science has shown a BRCA mutation is the single biggest risk factor for breast cancer. If your family history includes any of the following, you may want to consider genetic counseling and testing:
- You're a female who was diagnosed with breast cancer before the age of 50
- You’re a male who was diagnosed with breast cancer or you have a close male relative who was diagnosed with breast cancer
- You have a mother, sister, daughter, grandmother or aunt who had breast cancer before age 50 or ovarian cancer at any age
- You have three relatives on the same side of the family who were diagnosed with breast cancer at any age
