Atherosclerosis
Find a doctorAtherosclerosis occurs when arteries become narrow and less flexible, restricting blood flow. Atherosclerosis increases your risk for heart attacks, strokes and other health problems. At Atrium Health Floyd and Harbin Clinic, we offer advanced treatments for all types of atherosclerosis.
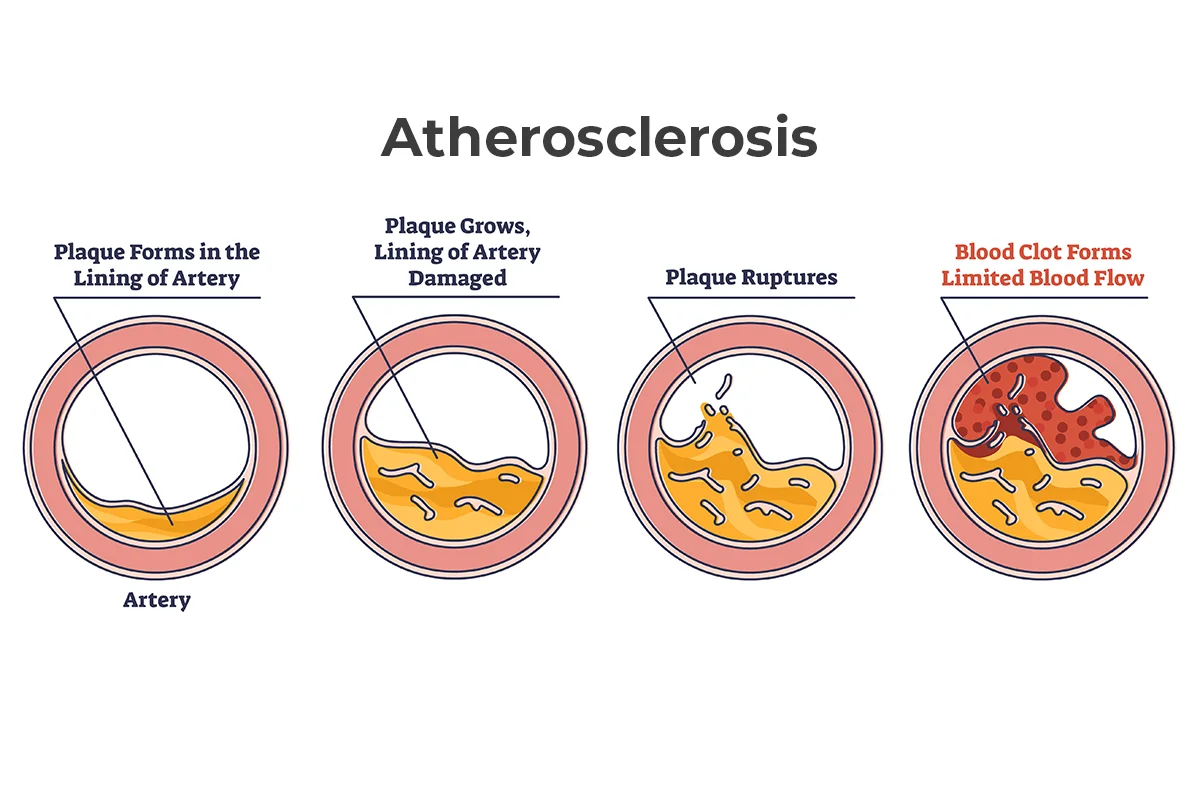
Four steps in the progression of atherosclerosis from plaque forming in the artery to a blocked artery with a blood clot and limited blood flow.
What is atherosclerosis?
Atherosclerosis is the medical term for hardening of the arteries. Your arteries carry oxygen-rich blood from your heart to the rest of your body.
Atherosclerosis can affect any artery in your body. It occurs when cholesterol, fat and other substances form deposits (plaque) inside the walls of an artery. This plaque buildup means there’s less room for blood to flow through. The affected artery becomes narrow and stiff.
Blood clots can form in affected arteries, causing a stroke. In severe cases, plaque can completely block an artery, stopping blood flow and causing a heart attack.
Causes of atherosclerosis
Atherosclerosis may result from damage to the inside layers of an artery wall. This damage may occur as early as childhood. Plaque deposits stick more easily to the damaged area. Over time, the plaque hardens and narrows the artery.
Certain conditions can damage and harden arteries, including:
- Diabetes or insulin resistance
- High blood pressure (hypertension)
- High levels of low-density lipoprotein (LDL) cholesterol
- High triglycerides
- Inflammation from other diseases
- Obesity
- Tobacco use
Atherosclerosis symptoms
Atherosclerosis may not cause symptoms until an artery becomes very narrow or there’s a blockage. Symptoms can vary depending on the affected artery.
Atherosclerosis heart symptoms
Hardening of the coronary arteries, which supply blood to your heart, may cause:
- Chest pain (angina)
- Dizziness
- Fatigue
- Heart palpitations
- Nausea and vomiting
- Pain in your back, shoulders, neck or arms
- Shortness of breath
Atherosclerosis brain symptoms
Hardening of the carotid arteries, which supply blood to your brain, may cause:
- Dizziness
- Facial drooping
- Severe headaches
- Speech problems, such as slurred speech
- Vision changes
Atherosclerosis digestive symptoms
Hardening of the arteries that supply blood to your digestive system may cause:
- Abdominal cramps, especially after eating
- Bloating
- Diarrhea
- Nausea and vomiting
- Unintended weight loss
Atherosclerosis kidney symptoms
Hardening of the renal arteries, which supply blood to your kidneys, may cause:
- Frequent urination or urinary problems
- Headaches
- High blood pressure that’s difficult to treat
- Itchy, dry skin
- Loss of appetite
- Nausea and vomiting
- Swelling
- Unintended weight loss
Atherosclerosis lower body symptoms
Hardening of the peripheral arteries, which supply blood to your limbs, may cause:
- Burning, tingling or numbness in the affected limb
- Cold feet or hands
- Discoloration or reddening of skin
- Muscle pain that makes it difficult to walk (intermittent claudication)
- Wounds or skin infections that are slow to heal
Atherosclerosis types
The type of atherosclerosis depends on the affected artery:
- Carotid artery disease affects the carotid arteries in your neck.
- Coronary artery disease (CAD) affects the coronary arteries.
- Mesenteric ischemia affects arteries that carry blood to your intestines.
- Peripheral artery disease (PAD) affects the peripheral arteries.PAD most commonly affects legs and feet, but it can also affect arms and hands.
- Renal artery stenosis affects the renal arteries.
- Vertebral artery disease (VAD) affects the arteries that carry blood to the back of your brain.
Atherosclerosis diagnosis
Your doctor will ask about your symptoms and medical history to diagnose atherosclerosis. They will also listen to your arteries during a physical exam. An abnormal whooshing sound called a bruit may indicate poor blood flow due to plaque buildup.
To confirm a diagnosis, your doctor may order tests such as:
- Ankle-brachial index (ABI) to measure blood flow in your arms and legs
- Blood tests to measure blood sugar, cholesterol, triglycerides and C-reactive proteins
- Electrocardiogram (ECG or EKG) to record your heart’s electrical activity
- Imaging scans, such as angiogram, MRI, ultrasound or positron emission tomography (PET) scan, to check blood flow through arteries
- Stress test to see how your heart responds to exertion
Atherosclerosis risk factors
Certain health conditions and other factors may increase your chances of developing atherosclerosis. These risk factors include:
- Age over 45 (males) or 55 (females)
- Coronary heart disease
- Diabetes, metabolic syndrome or obesity
- Diet high in saturated fat, sugar and sodium
- Family history of early diagnosis of heart disease
- High levels of LDL cholesterol or triglycerides
- Hypertension
- Sedentary lifestyle
- Substance use disorder (addiction), including using tobacco
Complications of atherosclerosis
Atherosclerosis may increase your risk of other health conditions, such as:
- Aneurysm
- Arrhythmia
- Heart attack
- Heart failure
- Kidney disease
- Stroke
Atherosclerosis prevention
The following actions may help lower your chances of developing atherosclerosis. They can also improve your health if you already have atherosclerosis.
- Cut back on alcohol.
- Find healthy ways to manage stress.
- Manage health conditions like high blood pressure, high cholesterol and diabetes.
- Maintain a healthy weight through physical activity and a heart-healthy diet.
- Seek help to quit smoking or using other drugs.
Heart services
Personalized heart care from experts you trust
Get the MyAtriumHealth app
Get test results, message your provider & more.